ABOUT HYPOPARATHYROIDISM
Understanding the etiology and impact of hypoparathyroidism
Hypoparathyroidism (HPT) is a rare and complex endocrine disorder characterized by absent or inappropriately low levels of endogenous parathyroid hormone (PTH).1-3
The symptoms and complications of HPT can be severe and persistent, posing a threat to multiple organ systems. Chronic HPT may also affect patients’ emotional well-being and quality of life.4,5
Endogenous PTH is a key regulator of mineral homeostasis.1,2
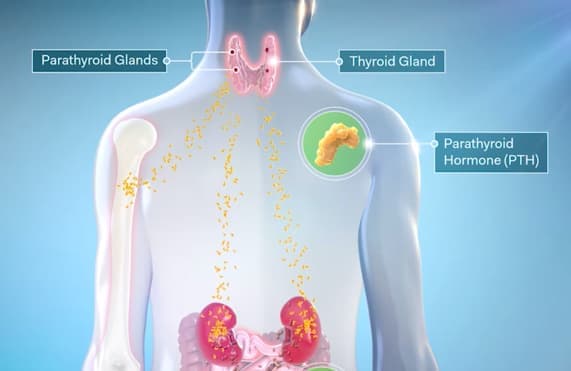
Endogenous PTH is secreted from the parathyroid glands in response to falling levels of circulating ionized calcium. When properly regulated, ionized calcium levels should not vary by more than 5%.6,7
Compromised PTH function leads to impaired mineral homeostasis, often resulting in1-3:
Decreased
serum calcium
Increased
serum phosphate
Increased
urinary calcium
Patients with HPT that is not adequately controlled can suffer from a high burden of illness.5
Burden of illnessIncidence and etiology
HPT affects
60,000- 115,000 people
in the United States.8
Surgery
Damage to the parathyroid glands during thyroidectomy, parathyroidectomy, or other neck surgeries is the most common cause of acquired hypoparathyroidism, accounting for ~75% of cases.9,10
75%
Postsurgical

25%
Other causes
Postsurgical HPT may resolve in a short time or become permanent. Chronic hypoparathyroidism can be diagnosed when low levels of endogenous PTH persist for ≥6 months.9,10
Autoimmune hypoparathyroidism
The second most common form in adults, autoimmune HPT may be isolated or part of an autoimmune polyglandular syndrome (APS).3
Genetic
Genetic mutations may impact parathyroid development, PTH synthesis, or resistance to PTH in the proximal renal tubule. HPT may feature in some complex congenital syndromes, such as DiGeorge syndrome. Excess accumulation of iron (thalassemia or hemochromatosis) or copper (Wilson’s disease) are other less common causes.3
Rare causes
Radiation treatment for cancers of the head or neck, or radioactive iodine treatment may interfere with parathyroid function. In some instances, hypoparathyroidism may be idiopathic in nature.3,9
Chronic HPT is associated with comorbidities that can affect several organ systems—including renal, neuropsychiatric, skeletal, cardiovascular, and ophthalmologic systems.4
RECOGNIZING COMPLICATIONS