Evaluation and Diagnosis
Hypoparathyroidism (HPT) evaluation and diagnosis
Clinical evaluation consists of patient history,
physical examination, lab tests, and imaging.
Evaluation of
Hypoparathyroidism
Patient history
Patient history should include a review for1,2:
- Thyroidectomy and/or parathyroidectomy.
- Surgery to other structures of the neck.
- Relevant family history of hypocalcemia or associated genetic disorders.
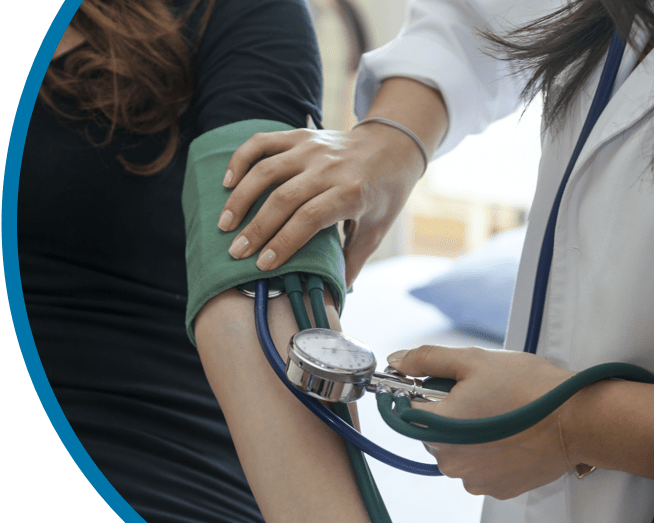
Physical exam
Assess for neuromuscular symptoms such as2:
Fatigue
Generalized
muscle weakness
Muscle cramping,
which may be painful
Bronchospasm
and wheezing
Neuromuscular irritability may be observed by testing for both (A) Chvostek’s and (B) Trousseau’s signs.1

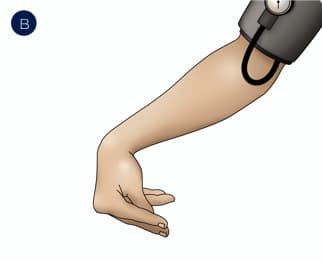
Neurologic signs of HPT may include paresthesia and numbness—especially around the mouth, fingers, or toes—and seizures or spells.2
An electrocardiogram may reveal prolongation of the QT interval caused by HPT-induced hypocalcemia.3
Labs
Lab tests include1:
- Serum total and ionized calcium
- Parathyroid hormone concentration
- Phosphate
- Magnesium
- BUN/creatinine
- 25-hydroxyvitamin D [25(OH) vitamin D]
Once a diagnosis is made, initial evaluation should include a 24-hour urinary calcium excretion, estimated or calculated GFR, and a biochemical stone risk profile if clinically warranted.1
Diagnosing hypoparathyroidism
HPT diagnosis is established by concurrent measurement of1:
- Albumin-corrected or ionized serum calcium below the lower limits of the normal range.
- Low or undetectable levels of parathyroid hormone (PTH) on at least 2 occasions.
as determined either by a 2nd- or 3rd-generation immunoassay separated by at least 2 weeks.1
TEST FOR HYPOCALCEMIA
Measure albumin-corrected or ionized serum calcium
on 2 occasions separated by at least 2 weeks.
TEST “WHOLE PTH” LEVELS
In the presence of hypocalcemia, measure PTH levels using
2nd- or 3rd-generation immunoassay on at least 2 occasions.
IF PTH LEVEL IS ELEVATED
Evaluate for pseudohypoparathyroidism
and secondary hyperparathyroidism.1
IF PTH LEVEL IS UNDETECTABLE OR INAPPROPRIATELY LOW
HPT is confirmed. Chronic HPT can be diagnosed when low levels of endogenous PTH persist for ≥6 months.1,4
Conventional management of HPT may involve dietary and oral calcium, active vitamin D, magnesium, thiazide diuretics, phosphate binders, and/or other dietary changes.1
Evaluating for adequate control in HPT patients on conventional therapy requires monitoring not only of serum calcium, but also of serum phosphate, calcium-phosphate product, and urinary calcium. Symptoms, quality of life, and comorbidities must also be observed.1